Implant Progress, Part 4
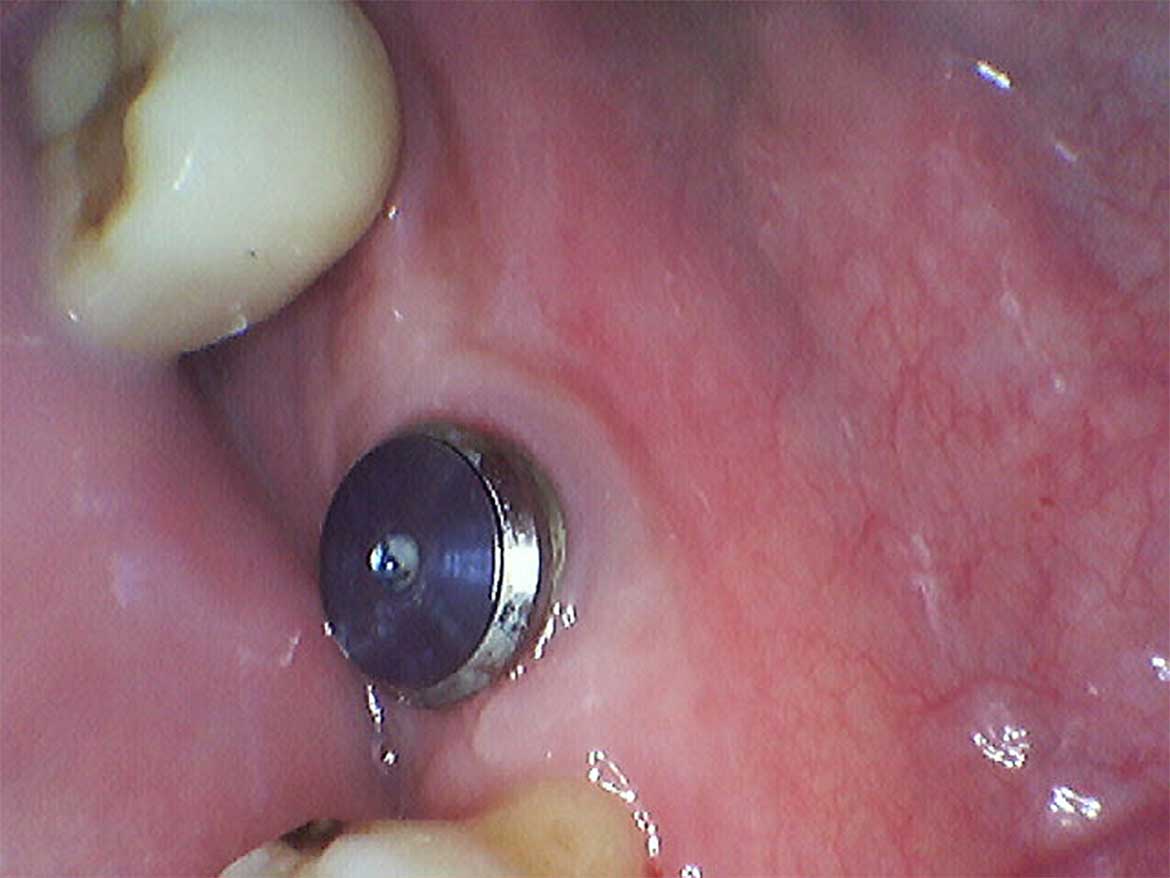
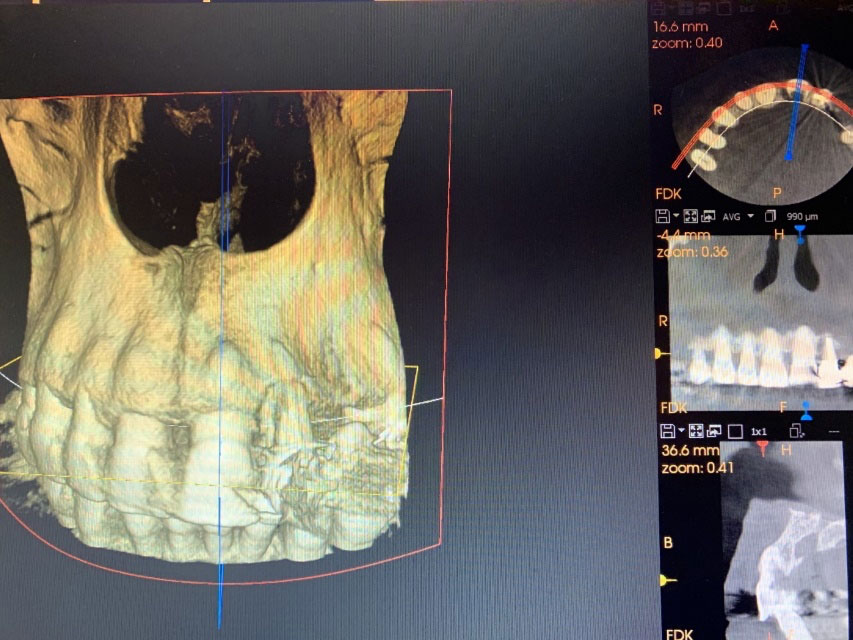
Earlier this August, I wrote a blog as a second instalment on an anterior implant case. The patient lost her upper left front tooth due to a severe cavity in the root (caused by external resorption). Subsequently, the tooth was extracted, and a Straumann BLX implant was surgically placed in the extraction socket. An exogenous bone graft (freeze-dried bone particles…